Clinical Update Forty-Three: Reduction of Air Emboli
Successful reduction of air emboli during open heart procedures
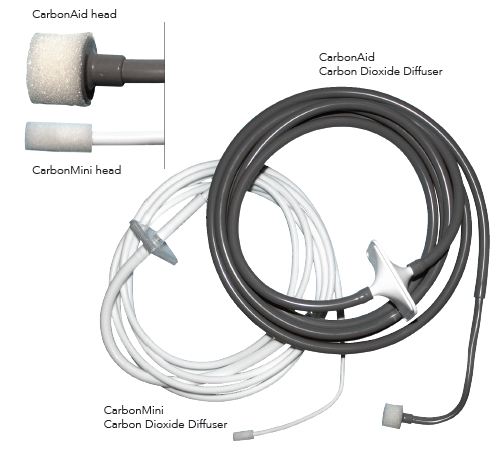
The CarbonAid® and CarbonMiniTM CO2 diffusion catheters protect patients by minimizing air emboli, by increasing bacteriostasis and by repelling particulate contamination during surgery.
The CarbonAid Carbon Dioxide (CO2) Diffuser is clearly a beneficial adjunct to open heart surgery–any time the heart is opened, especially for valve surgery, the advantage of a consistent, non-turbulent CO2 atmosphere for the heart is an obvious improvement for patient recovery because air microemboli are greatly reduced.1-4 This product is available in sizes for adult and pediatric surgery (Figure 1). The new “CarbonMini” size is useful in minimally invasive adult cases as well as pediatric procedures.1
Figure 1. CarbonAid and CarbonMini Carbon Dioxide (CO2) Diffusers
Neurological sequelae of cardiovascular surgery are devastating
Cognitive deficit after valve replacement surgery has been well documented and is irreversible in older patients.5-9 Studies have shown the benefit of efficient CO2 flooding during open heart surgery.9,10
Reduction of air emboli decreases operative time
Operative time that comes at a high cost per minute can be decreased by as much as 15 minutes per case if there are few or no air bubbles present after cardiac closure.4,10 CO2 insufflation of cardiac wounds using only a cannula is not nearly as effective as the CarbonAid diffuser.4 De-airing is not as complete due to turbulence created in the pericardial cavity when plain tubing is used (Figure 2).4
Figure 2.
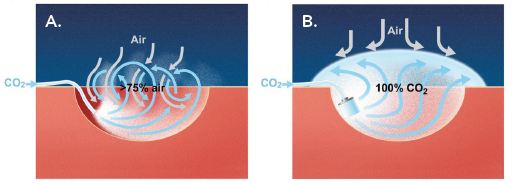
A. CO2 fed into a pericardial cavity with a simple tube creates turbulence that mixes regular air (up to 75%) with the infused CO2. B. The CarbonAid diffuser feeds CO2 in a non-turbulent manner creating a complete de-airing of the pericardial cavity and a protective layer of CO2 that may ensure reduction of microemboli, repel small particles and provide a bacteriostatic effect.1-4,11,12
Two additional benefits of proper CO2 diffusion for all cardiac cases
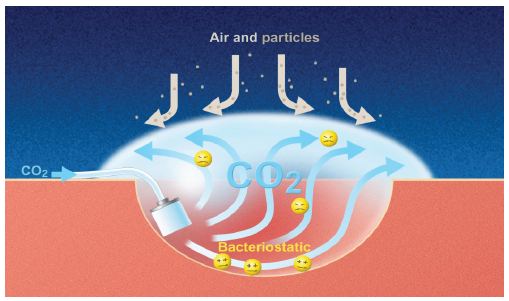
In addition to reduction of air emboli, two important benefits of proper CO2 diffusion are:
- Creation of a protective barrier against airborne particles from the surgical team/operating room ventilation (Figure 3)12,13
- AND the bacteriostatic effect of an improved CO2 atmosphere (Figure 3) may reduce infectious occurrences including endocarditis.11
These two benefits of the CO2 field result from use of the CarbonAid diffuser and apply to all cardiac cases, not just open heart procedures such as valves.
Figure 3. CO2 has bacteriostatic properties creating an unfavorable environment for growth.11 The protective environment of a CO2 atmosphere that is created by CO2 diffusion may repel particulate matter away from the pericardial cavity.12,13
Endocarditis reduction decreases hospital costs
Treatment of endocarditis is estimated to cost between $47,577 to $98,294.14,15 Use of the CarbonAid CO2 diffuser can reduce surgical infection thus offsetting its cost.
Below are important exerpts from published articles about proper CO2 diffusion:
Reduction of microemboli from cardiac wound insufflation with CO2 (de-airing):
“Thus, a mere decrease of the number of microemboli had a beneficial effect, wheras CO2 insufflation not only decreases the number of emboli but probably also decreases the harm they can do.” Svenarud, et al. 200410
De-airing (insufflation) of the cardiothoracic wound (or cavity) with a diffuser versus conventional open-ended tubing:
“This study showed that the gas-diffuser produced efficient de-airing of a cardiothoracic wound model at CO2 flows of ≥ 5 L/min, whereas an open-ended tube did not achieve this.” Svenarud, et al.16
“This study demonstrated that a carbon dioxide flow of 10 L/min the gas provided efficient air displacement (≤1% remaining air) in a cardiothoracic wound cavity.” Svenarud, et al.17
“There may be a solution to the problem with inefficient CO2 de-airing. First, the CO2 flow must be high enough to counteract diffusion with ambient air. Secondly the delivered CO2 must have a low velocity to avoid turbulent mixing with ambient air. Conventional open-ended tubes provided a poor and varying de-airing of the wound cavity model (18%-96% remaining air) . . . . The gas diffuser provided an almost complete de-airing of the model (<0.2% remaining air) at flows of 5 to 10 L/min.” Persson and Van Der Linden4
Carbon dioxide has long been known to inhibit the growth of bacteria:
“To sum up, 100% CO2 significantly decreased the growth rate of S. aureus at body temperature. The inhibiting effect of CO2 increased exponentially with the duration of the exposure. The bacteriostatic effect of CO2 could help to explain the low infection rates after laparoscopic procedures.” Persson, et al.18
Reduction of airborne-particles in the cardiac wound:
“In conclusion, intraoperative wound ventilation with CO2 in the cardiothoracic wound using a gas diffuser may not only prevent air embolism, but may also significantly reduce the risk of airborne contamination and postoperative wound infection in cardiac surgery.” Persson and van der Linden19
“This study provides supportive evidence . . . that intraoperative wound ventilation may be a simple complement to prevent direct airborne contamination.” Persson and van der Linden12
A less turbulent CO2 atmosphere provides your patients with the best opportunity for the shortest operative time, reduced neurological complications, reduction of airborne contamination and less infection with the CarbonAid and CarbonMini CO2 diffusion catheters.
References
- Prevent air embolism during open-heart surgery. Cardia Innovation brochure, Stockholm, Sweden, 2012
- van der Linden J, Persson M, Svenarud P. Carbon dioxide insufflation on the number and behavior of air microemboli in open-heart surgery—response. Circulation 2004;110(5):E55-56
- Persson M, Svenarud P, van der Linden J. What is the optimal device for carbon dioxide de-airing of the cardiothoracic wound and how should it be position? J Cardiothorac Vasc Anesthesia 2004;18(2):180-84
- Persson M, van der Linden J. De-airing of a cardiothoracic wound cavity model with carbon dioxide: theory and comparison of a gas diffuser with conventional tubes. J Cardiovasc Vasc Anesthesia 2003;17(3):329-35
- Hogue CW, Fucetola R, Hershey T, et al. The role of postoperative neurocognitive dysfunctionon quality of life for postmenopausal women 6 months after cardiac surgery. Anesth Analg 2008;107(1):21-28
- Gao L, Taha R, Gauvin D, et al. Postoperative cognitive dysfunction after cardiac surgery. Chest 2005;128(5):3664-70
- Juolasmaa A, Outakoski J, Hirvenoja R, et al. Effect of open heart surgery on intellectual performance. J Clin Neuropsychol 1981;3(3):181-97
- Zimpfer D, Czerny M, Kilo J, et al. Cognitive deficit after aortic valve replacement. Ann Thorac Surg 2002;74(2):407-12
- Martens S, Neumann K, Sodemann C, et al. Carbon dioxide field flooding reduces neurologic impairment after open heart surgery. Ann Thorac Surg 2008;85(2):543-47
- Svenarud P, Persson M, van der Linden J. Effect of CO2 insufflation on the number and behavior of air microemboli in open-heart surgery. Circulation 2004;109(9):1127-32
- Persson M, van der Linden J. Intraoperative CO2 insufflation can decrease the risk of surgical site infections. Medical Hypotheses 2008;71(1):8-13
- Persson M, van der Linden J. Wound ventilation with ultra-clean air for prevention of direct airborne contamination during surgery. Infection Control and Hospital Epidemiology 2004;25(4):297-301
- van der Linden J, Persson M. A guaze sponge cannot act as a gas diffuser in cardiac surgery when it gets wet. J Thorac Cardiovasc Surg 2003;125(5):1178-79
- Goodwin AT, et al. Outcomes in emergency redo cardiac surgery: cost, benefit and risk assessment. Interact Cardiovasc Thorac Surg 2003;2:227-30
- Caviness AC, et al. A cost-effectiveness analysis of bacterial endocarditis prophylaxis for febrile children who have cardiac lesions and undergo urinary catheterization in the emergency department. Pediatrics 2004;113:1291-96
- Svenarud P, Persson M, van der Linden J. Intermittent or continuous carbon dioxide insufflation for de-airing of the cardiothoracic wound cavity? An experimental study with a new gas-diffuser. Anesthesia & Analgesia 2003;96(2):321-27
- Svenarud P, Persson M, van der Linden J. Efficiency of a gas diffuser and influence of suction in carbon dioxide deairing of a cardiothoracic wound cavity model. J Thorac Cardiovasc Surg 2003;125(5):1043-49
- Persson M, Svenarud P, Flock J-I, et al. Carbon dioxide inhibits the growth rate of Staphylococcus aureus at body temperature. Surgical Endoscopy 2005;19(1):91-94
- Persson M, van der Linden J. A simple system for intraoperative antiseptic wound ventilation. J Hospital Infection 2003;55(2):152-53
On-X aortic and mitral valves are FDA approved. Not all On-X valve models are available in all markets.
CAUTION: Federal law restricts this device to sale by or on the order of a physician. Refer to the Instructions for Use that accompany each valve for indications, contraindications, warnings, precautions and possible complications. For further information, visit www.onxlti.com.
Headquarters and Manufacturing Facilities: 1300 East Anderson Lane, Building B Austin, Texas 78752 U.S.A.
Telephone: (512) 339-8000 – Facsimile: (512) 339-3636 – www.onxlti.com – onx@onxlti.com
010006 220 012213 © 2013 On-X Life Technologies, Inc.


